Diabetes, a disease affecting millions worldwide, is notorious not just for its direct impact on blood sugar levels but also for its potential to wreak havoc on various body systems — most notably, perhaps, the eyes. Diabetic eye disease encompasses a group of eye problems that people with diabetes may face as part of their journey with the condition. This can include diabetic retinopathy, diabetic macular edema (DME), cataracts, and glaucoma. Each of these conditions has the potential to cause significant vision impairment or even blindness if not diagnosed and treated early. Recognizing the symptoms of diabetic eye disease is the first crucial step toward prevention, timely intervention, and preserving vision.
Diabetic Eye Disease: A Closer Look
Before diving into the symptoms, it’s essential to understand what we’re dealing with when we talk about diabetic eye disease. At its core, the issue revolves around the damage high blood sugar levels can inflict on the blood vessels in the retina, leading to conditions like diabetic retinopathy and DME. Cataracts and glaucoma also occur at an earlier age and progress more rapidly in individuals with diabetes, adding layers of risk to an already complex situation.

Diabetic Retinopathy
Diabetic retinopathy is the most common eye complication associated with diabetes. It occurs when high blood sugar levels cause damage to the blood vessels in the retina. These vessels can swell, leak, or close, stopping blood from passing through. In some cases, abnormal new blood vessels grow on the retina, which can lead to further complications, including vision loss.
Diabetic Macular Edema (DME)
DME is a consequence of diabetic retinopathy and involves swelling in an area of the retina called the macula, which is crucial for sharp vision. This swelling occurs when fluid leaks into the macula, causing blurred vision or vision loss.
Cataracts
While cataracts can affect anyone, people with diabetes are more likely to develop this condition at a younger age. Cataracts cause the eye’s lens to cloud, obscuring clear vision.
Glaucoma
Glaucoma affects the optic nerve and leads to increased pressure inside the eye. Over time, this pressure can damage the optic nerve severely, resulting in vision loss.
Recognizing the Symptoms
One of the most insidious aspects of diabetic eye disease is that in its early stages, there may be no symptoms. This silent progression emphasizes the importance of regular eye exams for individuals with diabetes. However, as the diseases progress, symptoms may become apparent.
Symptoms of Diabetic Retinopathy and DME
- Blurred Vision: Initially, it may come and go, but it can progressively worsen.
- Floaters: These are spots or dark strings floating in your vision.
- Blank or Dark Areas: You may notice portions of your vision are missing.
- Color Impairment: Colors appear washed out or different than usual.
- Vision Loss: Over time, significant vision loss can occur, potentially leading to blindness.
Symptoms of Cataracts
- Clouded, Blurred, or Dim Vision: Like looking through a foggy window.
- Increased Difficulty with Vision at Night: Especially while driving.
- Sensitivity to Light and Halos Around Lights: Lights may appear too bright or glaring.
- Fading or Yellowing of Colours: Colours seem faded or not as vibrant as before.
- Double Vision in a Single Eye: This can occur in advanced stages.
Symptoms of Glaucoma
- Patchy Blind Spots: These can be in your peripheral or central vision and often in both eyes.
- Tunnel Vision: In advanced stages, central vision may remain, but peripheral vision is lost.
- Severe Headache, Eye Pain: This can be accompanied by nausea and vomiting.
- Halos Around Lights: Vision of halos around lights, especially in low light.
Early Detection and Management: A Ray of Hope
The key to combating diabetic eye disease lies in early detection and effective management. For individuals living with diabetes, this means adhering to a regimen of regular comprehensive dilated eye exams. Early intervention can dramatically alter the course of these conditions, slowing their progression, or even reversing damage in some cases.
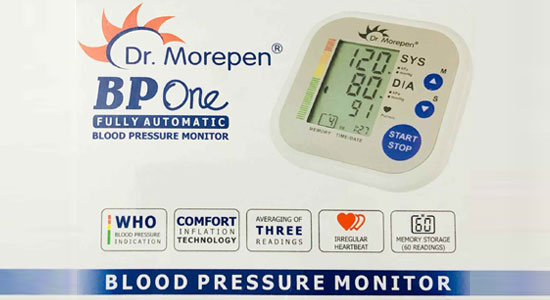
Living with Diabetes: A Focus on Eye Health
Beyond regular eye exams, managing blood sugar levels, blood pressure, and cholesterol are vital strategies in preventing the onset or worsening of diabetic eye diseases. Lifestyle modifications, including a healthy diet, regular exercise, and smoking cessation, play a crucial role in overall diabetes management and, by extension, eye health.
The Role of Technology and Treatment
Advancements in medical treatments and technologies, such as laser therapy, injectable medications (including anti-VEGF treatment), and surgical options, offer hope and practical solutions for managing diabetic eye disease. Consultation with medical professionals, including endocrinologists and ophthalmologists specializing in diabetic eye care, is essential for navigating these options.
Conclusion
Diabetic eye disease represents a significant risk for individuals living with diabetes but recognizing the symptoms and understanding the importance of early detection can lead to effective management and preservation of vision. As research advances and awareness grows, the hope is that more people will take the necessary steps to protect their eye health, ensuring that they and their loved ones can look forward to a brighter, clearer future.
Hey there! I’m a self-proclaimed Twitter addict and an unapologetic coffee lover.